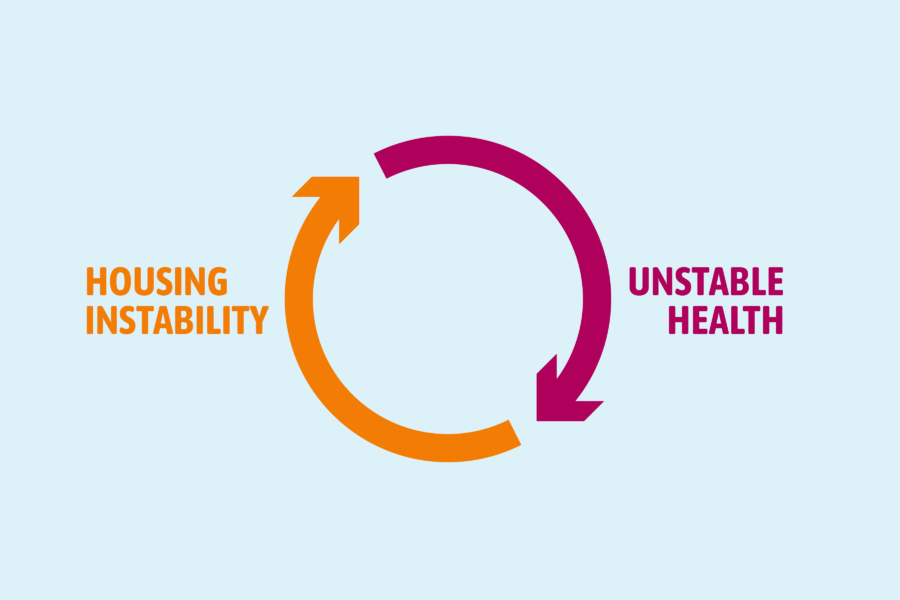
Homelessness is a public health crisis. Experiencing homelessness makes it harder to become and remain healthy. Research has shown that the lack of safe, affordable, and decent housing can negatively impact a person or family’s health and well-being. Individuals and families who forgo healthy food or medicine to pay high housing costs may experience poor health outcomes.
Homelessness affects both physical and mental health. In addition, experiencing homelessness makes accessing health care difficult. As a result, people experiencing homelessness are generally sicker than their housed counterparts and more prone to death.
Reducing and preventing homelessness does not just impact the health and well-being of people experiencing and at risk of homelessness; the positive impacts ripple outward, yielding lower health care costs and healthier communities. The cross-system work to reduce homelessness, create more affordable housing, and prevent housing instability ultimately impacts the health and well-being of entire communities and, by extension, makes the whole state healthier.
Given the relationship between housing and health, state public health agencies, officials, and policymakers are well-positioned to bring new resources, ideas, ways of working, and capacity to the collaborative effort to make homelessness rare and brief.
Community Solutions developed the State Public Health & Homelessness Playbook for state public health officials, homelessness and housing advocates, and state policymakers who want to learn more about how state public health agencies and programs can proactively support efforts to reduce and prevent homelessness.
There is no singular or right way for state public health departments to participate in what should be a whole-of-government effort to prevent and reduce homelessness.
The playbook includes a myriad of examples showcasing innovative, dynamic partnerships between state public health departments and the homeless response system to improve the health and well-being of people experiencing homelessness.
Here are five key learnings from the playbook:
1) States can play an important role in solving homelessness.
While states do not have an explicit role in the existing homeless response system or funding paradigm, they do have considerable influence over various policy arenas that impact the homeless service system, such as land-use policy, health care funding (specifically Medicaid), criminal justice policy, and affordable housing financing. States can and should proactively leverage these resources and policymaking arenas to solve homelessness by developing and preserving affordable housing, investing in data-driven, coordinated programming to reduce homelessness statewide, awarding funding to support innovation and flexible service delivery, and championing the use of Housing First programming in the state, to name a few opportunities.
2) Shared real-time, person-centered data is the critical foundation that facilitates care coordination between public health and homeless response systems.
State public health agencies have a unique ability to lead cross-sector efforts to integrate and share real-time, person-centered data that details who is experiencing homelessness throughout the state. This information has traditionally only been known to officials in the city or county that a person is living in or limited by privacy or system integration challenges. Without shared data, the health and homeless response systems cannot properly coordinate care for individuals and drive the systems-level changes that can improve housing and health outcomes at the population level. Data coordination and integration are the keys to creating effective and responsive public policy solutions that impact population and community health while providing monitoring and evaluation mechanisms to drive future policy and programming.
3) State public health departments can bridge the gap between local homeless service delivery and population health by proactively defining a role within the homeless response system.
State public health departments can expand their role in ending and preventing homelessness by designing roles tasked with being proactive partners to the homeless response system. This dedicated capacity allows for expanded participation in joint programming, data sharing or matching, and coordinated cross-sector case conferencing. Additionally, public health departments can use their special powers, such as the ability to declare a public health crisis, to help build momentum to reduce and prevent homelessness and garner new resources to assist the homeless response system.
4) State public health agencies can help finance affordable and supportive housing.
Stable, affordable housing is the foundation for good health. Housing provides privacy, safety, and a reliable, consistent place to rest and recuperate. Housing can also reduce health care and social service costs. Given the relationship between health and housing, state public health departments can promote ways to increase the available stock of affordable and supportive housing by leveraging state Medicaid funding and public health data.
5) Medicaid programs and waivers are exciting opportunities for states to pilot and test innovative approaches to projects that both promote well-being and enhance access to funding and reimbursement supports to promote housing stability.
State public health departments can play a critical role in crafting solutions that meet the complex needs of people experiencing homelessness. As the average age of the population experiencing homelessness continues to creep above fifty years old, state public health departments can help create housing supports and facilities that can meet the needs of this vulnerable population, such as respite care for individuals recovering from medical care and shelters aimed at supporting and healing those individuals with complex medical cases.