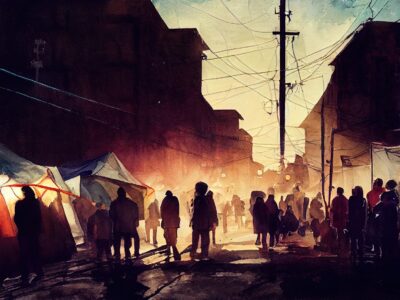
The 2023 Annual Homelessness Assessment Report (AHAR) found that on a single night in January 2023, approximately 653,100 Americans were experiencing homelessness across the United States.
Homelessness affects both physical and mental health and makes accessing health care difficult. As the National Health Care for the Homeless Council asserts, being unhoused “creates new health problems and exacerbates existing ones.”
Medicaid provides health coverage to millions of Americans, including eligible low-income adults, children, pregnant women, elderly adults, and people with disabilities. In the last decade, Medicaid has been championed as a strong resource and lever for individuals experiencing homelessness or at risk of it. In the 14 years since coverage options expanded under the Affordable Care Act, an increasing number of states have explored health-related social needs and social determinants of health mechanisms that linked their most vulnerable citizens to critical services.
As each state varies in their population, demographics, and governance structure, these differences can be leveraged to meet the needs of people experiencing homelessness and expand the health care services available through the homeless response system. States have the flexibility to customize their programming and design service provision that meets their citizens’ specific needs.
As Built for Zero listened to community members and their needs, there seemed to be a critical voice missing in the design and research around these innovative Medicaid and Housing programs: the Continuum of Care (CoC) staff.
This survey was designed to explore a sample of CoC staff’s understanding, expertise, and challenges with Medicaid and its related programs.
Most often, CoC staff and frontline workers have a deep understanding of the needs of their local population and the types of services most in-demand and impactful to these individuals.
Survey Overview
- 66 complete responses and 16 partial responses
- 81% completion rate overall
- Respondents represent 48 different CoCs from 27 different states, 22 of which have expanded Medicaid, and five which have not.
- 33% of respondents were at the Director level in their CoC, while 39% were at the programmatic or project level. The remaining 28% were either Coordinated Entry, Data/HMIS, or Outreach Staff.
Key Findings
- Most CoC respondents see Medicaid as a powerful program that can benefit their work in some form or another.
- Partnerships exist between Medicaid teams or Managed Care Organizations and CoCs. Some even include joint case conferencing or data integration.
- There’s still a significant gap in perceived value and understanding when it comes to these Medicaid programs.
- Data integration is a common starting point, but it’s complex, technical, and burdensome, so there needs to be a clear goal.
- Waivers that are connected to housing supports or unhoused populations aren’t well understood or leveraged by CoCs.
Key Recommendations
- Expanded education and training for CoCs on Medicaid and Managed Care Organizations (MCOs)
- Exploration of models for MCOs and Medicaid to join case conferencing led by CoCs, either with or without data integration supports.
- Inclusion of CoC Leadership at Medicaid roundtables, waiver design working groups, and other cross-sector discussions.
- Increased dissemination of evidence and evaluations from existing waivers, pilot programs, and tests for shared learnings.